FAO and the mpox outbreak
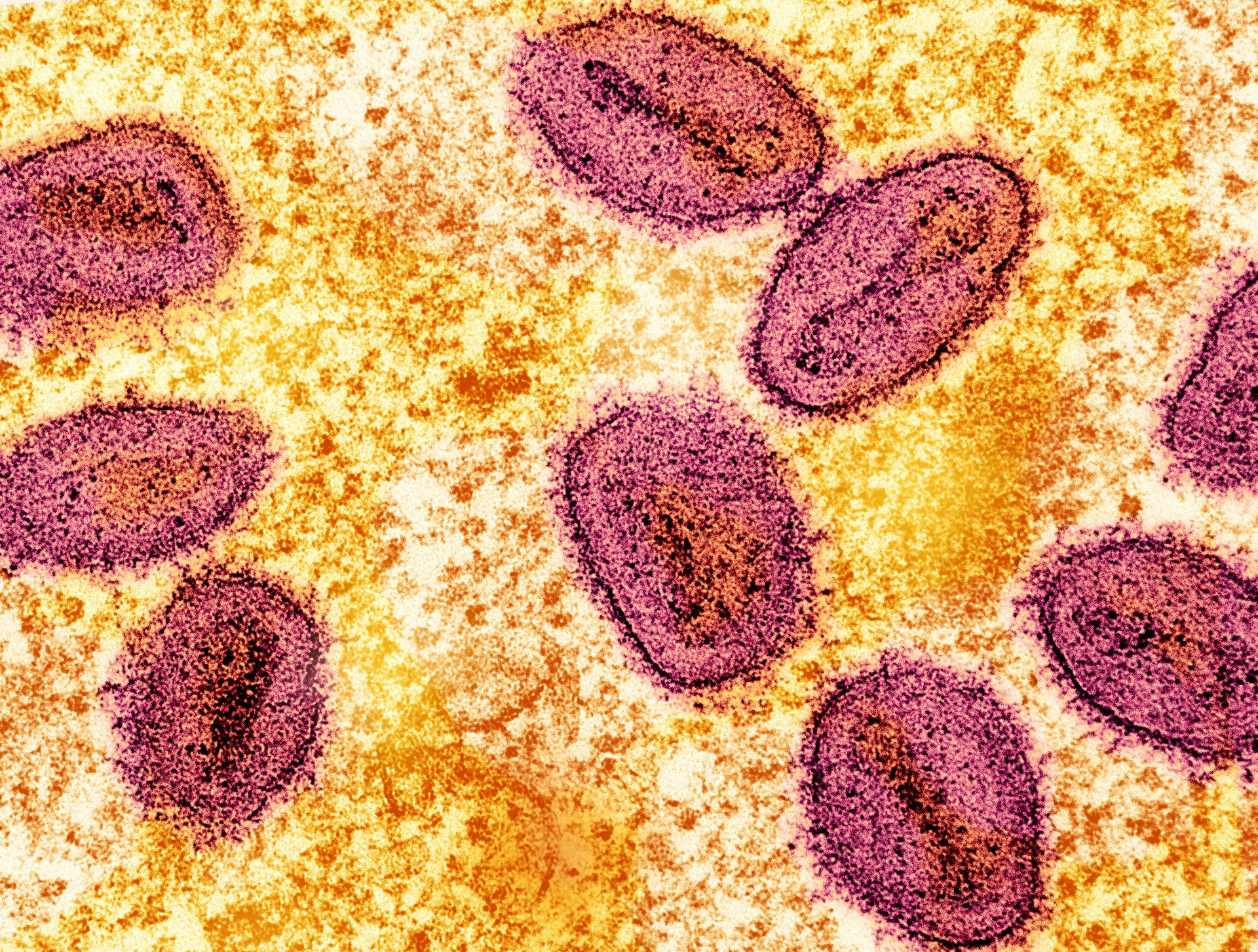
Mpox is a viral zoonotic disease that occurs primarily in tropical rainforest areas of Central and West Africa and is occasionally transmitted to other regions. Two different clades (or strains) exist: clade I and clade II.
In endemic areas, the virus is thought to be maintained through circulation among susceptible mammals, namely wild rodents such as squirrels and rats, with occasional spill-over to primates and humans.
Infected animals may be asymptomatic, meaning they show no symptoms of mpox, especially species suspected of being reservoirs (i.e. rodents). Other mammals, such as monkeys and great apes, show skin rashes similar to those experienced by humans.
How is mpox transmitted?
Transmission of MPXV can occur when a person or susceptible animal comes into contact with the virus from an animal, human, or materials contaminated with the virus. The virus enters the body through skin lesions (not necessarily visible to the naked eye), respiratory tract, or mucous membranes.
Animal-to-human (zoonotic) transmission can occur from direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals, through bites or scratches, or during activities such as hunting, skinning, or trapping of infected animals. Eating inadequately cooked meat and other animal products is a risk factor, as is living in or near forested areas, due to indirect or low-level exposure to infected animals.
Human-to-human transmission can result from close contact with respiratory secretions, body fluids, skin lesions of an infected person or recently contaminated objects such as bedding. During the multi-country outbreak that began in 2022, the virus mostly spread through sexual transmission. Transmission can also occur via the placenta from mother to foetus (which can lead to congenital mpox) or close contact during and after birth.
Spillback of the virus from infected humans to animals is a possibility that could lead to the virus becoming endemic in new geographic areas. Evidence of human-to-dog transmission of mpox has been documented. Settings where humans and captive apes and primates interact (such as zoos, circus facilities, and animal parks) also provide opportunities for transmission to susceptible animal species.
What is FAO doing?
FAO is working with its partners, through the One Health approach, to gather the latest scientific information and evidence from various sources, including FAO-EMPRES Global Early Warning System (GLEWS) to support science-based decisions on prevention and mitigation of the risk of mpox in Member countries.
The ongoing events were discussed with WOAH and WHO through the Global Early Warning System for health threats and emerging risks at the human–animal–ecosystems interface (GLEWS+).
Since 1 October 2022, FAO, through its Emergency Centre for Transboundary Animal Diseases (ECTAD), has been implementing a two-year project to support the governments of the Democratic Republic of the Congo and the Federal Republic of Nigeria. Through this initiative FAO has helped to enhance national capacities to detect mpox in susceptible animal species using a One Health approach.
Recommended actions for surveillance in animal populations and prevention of infection spillback from humans
Because mpox has a zoonotic origin, its effective management warrants application of the One Health approach. While supporting the efforts of the World Health Organization (WHO) and countries in preventing further spread of mpox at the human-animal interface, FAO recommends the following actions for community awareness and surveillance in animals:
- Veterinary services should be included in joint outbreak investigations promptly when animal exposure is suspected, following procedures developed as part of national contingency plans.
- For all countries experiencing cases of human infection with MPXV, One Health epidemiological investigation is recommended by testing animals exposed to MPXV infected humans to exclude their being infected - particularly in cases of close direct and prolonged contact with the infected person. Testing should be prioritised in species known to be susceptible to infection though, due to the lack of knowledge of all susceptible species, testing in other species may be indicated. Similarly, testing should focus primarily on animals that are also showing signs of disease, though subclinical infection is also possible and needs to be considered in outbreak investigation.
- People who are suspected or confirmed to be infected with MPXV should avoid close direct contact with animals, including domestic animals (such as cats, dogs, hamsters, ferrets, gerbils, etc.), livestock and other captive animals, as well as wildlife.
- Ensure that all waste, including medical waste is appropriately disposed of, ensuring that it is not accessible to rodents and other scavenger animals.
- Raise awareness of the public on the modes of transmission of MPXV, including the risks posed by the processing and consumption of meat from wild animals.
- Practice basic personal hygiene measures, in particular regular handwashing before and after handling animals.
- Personal protective measures should always be followed by veterinary personnel and animal care workers when dealing with sick animals, including animals that could potentially be infected with MPXV.
- If feasible, pet rodents and other susceptible animals in households with infected people should be quarantined for a period of 21 days to minimise their risk of infection.
- Response measures following detection of positive cases in animals should be based on country-specific risk assessment.
- As a matter of precaution, contact your veterinarian for guidance if you are concerned about transmission to animals under your care.
Situation updates on the surge of mpox infections in humans
- WHO Multi-country outbreak of mpox, External situation report #35 - 12 August 2024
- PAHO Epidemiological Alert Mpox (MPXV clade I) - 8 August 2024
- African region faces an unprecedented surge in mpox cases
